burning love
Localized Provoked
Vulvodynia
Nutritional Supplements Help Improve Vulvodynia (Formerly Vulvar Vestibulitis)
By Ladd McNamara, M.D.
Please read medical disclaimer below, and consult your health care professional prior to acting upon information provided in the article, protocol, or website.
Discussion
Vulvar vestibulitis syndrome, more recently known as Localized Provoked Vulvodynia, or vestibulodynia (LPV), is a little known condition that afflicts many women, especially women who believe they suffer from near constant yeast infections. LPV is a chronic vulvar vestibular burning and pain with intercourse that initially persists longer than three months. Vulvar vestibulitis, or LPV, is characterized by vaginal rawness, burning, irritation, or any other type of pain associated with touch or sexual intercourse that is not attributable to any other cause, such as infections or consequence of any treatment.
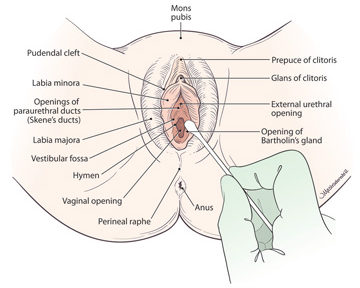
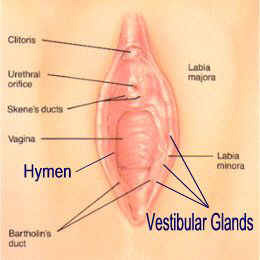 The delicate area surrounding the opening of the vagina is known as the vulvar vestibule. The vulvar vestibule is located inside the labia minora, but outside the vaginal hymen, or hymenal remnant, and is technically a part of the vulva. Tender localized areas are usually found around the opening of the Bartholin’s ducts, and in-between posteriorly. Sometimes the tenderness is around the vestibular glands as well.
The delicate area surrounding the opening of the vagina is known as the vulvar vestibule. The vulvar vestibule is located inside the labia minora, but outside the vaginal hymen, or hymenal remnant, and is technically a part of the vulva. Tender localized areas are usually found around the opening of the Bartholin’s ducts, and in-between posteriorly. Sometimes the tenderness is around the vestibular glands as well.
The lining of the vaginal wall does not have pain or touch receptors like the vestibule of the vulva, which is very sensitive to both touch and pain. A woman with a yeast infection does not feel burning or itching in the vagina, but rather in the vulvar vestibule.
Depending upon severity, women with localized provoked vulvodynia (LPV) usually may not be able to tolerate wearing pants, riding a bicycle, insertion of tampons, and sexual intercourse. The rawness associated with sex may progress from just “dryness” to severe burning, and without treatment can affect a woman and her intimate relationship for years.
Localized provoked vulvodynia may be confused for a yeast infection that never completely goes away, or one that recurs within a week or less after treatment for yeast. Certainly, yeast can and does worsen the symptoms of localized provoked vulvodynia, but the root problem is not yeast, it is a hypersensitivity of the nerve endings within the vestibule.
 Localized provoked vulvodynia (LPV) is a difficult condition to manage, with no real good treatment options offered, but there is hope. Right now, the best treatment is whatever works. (1) Although the results vary, I have seen a good deal of success among women suffering from LPV who follow my guidelines and supplement protocol.
Localized provoked vulvodynia (LPV) is a difficult condition to manage, with no real good treatment options offered, but there is hope. Right now, the best treatment is whatever works. (1) Although the results vary, I have seen a good deal of success among women suffering from LPV who follow my guidelines and supplement protocol.
Vulvar vestibulitis is a type of vulvodynia, which means “painful vulva.” When I practiced medicine, most doctors had not heard of vulvar vestibulitis, as it was not a well-known diagnosis. In the mid-to-late 1990s, vulvar vestibulitis syndrome was only known by a few specialists, including myself. In 2015, the terminology was standardized, and the name of vulvar vestibulitis syndrome was changed to localized provoked vulvodynia. I use both names in this article since many people still know it as vulvar vestibulitis, but it is now time to use the term, localized provoked vulvodynia.
In the mid-1990s, I became familiar with “vulvar vestibulitis” because a few patients complained of this strange burning pain and sex with intercourse that I could not initially seem to adequately treat. They clearly did not have a vaginal infection, and if I did treat for yeast anyway, they got better during the treatment, and a day or two after stopping the anti-fungal medication, but the burning and the pain quickly returned.
 Then, I recommended supplements, including high-dose grape seed extract. Immediately, I had the first 3 patients experience great results, 2 of whom had complete resolution of the pain and burning. As word spread to vulvodynia support groups, I treated more patients, with varying degrees of success. Through trial and error, I eventually developed my current protocol and guidelines for managing this frustrating syndrome.
Then, I recommended supplements, including high-dose grape seed extract. Immediately, I had the first 3 patients experience great results, 2 of whom had complete resolution of the pain and burning. As word spread to vulvodynia support groups, I treated more patients, with varying degrees of success. Through trial and error, I eventually developed my current protocol and guidelines for managing this frustrating syndrome.
I soon had patients coming from around the country and abroad to seek my care. I spoke at the National Vulvodynia Association events. I coached other doctors in treating according to my protocols, and now I have made my protocol available for others, here.
I developed non-invasive treatments for this condition in hopes of patients avoiding laser treatments or surgical excision of the vulvar vestibule. However, in severe cases that did not respond to my protocol, then excision of the posterior vestibule was deemed necessary. Long-term results are generally good with this procedure. (2, 3)
Toxic Exposure
Localized provoked vulvodynia appears to be on the rise, very likely due to our increasing exposure to toxic chemicals in our food, water, home, workplace, and environment. Avoiding toxic chemicals is very difficult, mostly because of our general lack of awareness to what it is we are being exposed at any given time.
 Due to my patients’ experience, I concluded that chlorine bleach (swimming pool, underwear washed with bleach), and bleached products (toilet paper, feminine hygiene products, etc.) exacerbates the burning and pain of LPV. Chlorine seems to be a major irritant that worsens burning and pain in women with this condition, and it is not only found in pools, but in the home water supply, and within bleach-whitened toilet paper and feminine hygiene products. Avoiding chlorine is an important management strategy.
Due to my patients’ experience, I concluded that chlorine bleach (swimming pool, underwear washed with bleach), and bleached products (toilet paper, feminine hygiene products, etc.) exacerbates the burning and pain of LPV. Chlorine seems to be a major irritant that worsens burning and pain in women with this condition, and it is not only found in pools, but in the home water supply, and within bleach-whitened toilet paper and feminine hygiene products. Avoiding chlorine is an important management strategy.
Pesticides, phthalates, dioxins, BPAs, etc., are xenoestrogens and/or endocrine disruptors and associated with endometriosis, premature ovarian failure, polycystic ovarian failure, and many other dysfunctions and disorders. (4 – 7) It is not so difficult to assume that these chemicals affect the hormone-sensitive tissues of the vulvar vestibule and may cause LPV.
Dioxins are found everywhere around the world, in our food, water, and air. Since dioxins are not broken down by bacteria, they persist in our environment for long periods of time, making them “persistent organic pollutants.” The two biggest sources of dioxin are the burning of plastics and chlorine bleach.
Dioxins get into the air from:
- Incineration of medical, municipal, and hazardous waste
- Facilities that use chlorine to make pesticides and PVC plastic
- Metal refining and smelting operations
Dioxins get into our food and water by:
 Airborne dioxins settle into soil, plants, and water.
Airborne dioxins settle into soil, plants, and water.- We eat animals and the plants, which are both contaminated. Dioxins accumulate and concentrate in fatty tissues.
Dioxin accumulates in body fat. With a half-life of over 7 years, it is eliminated slowly. It is important to reduce dioxin exposure as much as possible, though it is very difficult to do so. Avoiding chlorine bleach is a not as difficult as avoiding dioxin found in food.
There are feminine hygiene products and toilet paper that are not bleached, but are whitened with hydrogen peroxide, which are better alternatives to anything bleached with chlorine. I have found that certain toilet paper brands are worse than others, particularly because they leave behind more microscopic fibers laden with dioxins from bleaching.
Other chemicals that should be avoided as much as possible are chemical additives and some food preservatives, aspartame, GMO foods, caffeine, and alcohol. All these chemicals, damage cells throughout the body via the generation of molecules known as free radicals. Free radicals cause oxidative damage, which leads to inflammation and pain.
The Disorder and Diagnosis
The diagnosis of localized provoked vulvodynia (LPV), is made by history and confirmed with examination. The red areas are tender to touch with a Q-tip in specific areas of the vestibule, making diagnosis relatively easy.
The cause of LPV has not yet been positively identified. However as mentioned, exposure to dioxins, BPA’s, PCBs’, phthalates, and chlorine, along with many other chemicals may contribute to this condition. Currently, the diagnosis is made by meeting certain criteria, which include symptoms of pain with intercourse that persists for at least three months at the exclusion of other causes, such as infections, chemical sensitivities, skin disorders, hormonal changes, or consequences of medical procedures or treatments, e.g., chemo therapy.
 A thorough history, physical exam, cultures, and when appropriate, vulvar biopsies, should be done to diagnose candidiasis, trichomoniasis, bacterial vaginosis, post-herpetic neuralgia, and various vulvar dermatoses, such as lichen sclerosis, lichen planus, and contact dermatitis. However, when the diagnosis of localized provoked vulvodynia is clear, biopsies do not need to be performed.
A thorough history, physical exam, cultures, and when appropriate, vulvar biopsies, should be done to diagnose candidiasis, trichomoniasis, bacterial vaginosis, post-herpetic neuralgia, and various vulvar dermatoses, such as lichen sclerosis, lichen planus, and contact dermatitis. However, when the diagnosis of localized provoked vulvodynia is clear, biopsies do not need to be performed.
The pain is a burning pain that is felt when there is any pressure or stretching of the delicate vulvar tissues that surround the vaginal opening. Stretching the vaginal opening obviously occurs with sex, but also with gynecological exams, and in particular a speculum examination. A woman may feel that she is tearing. Inserting a tampon, prolonged sitting, and wearing tight pants can be painful.
Patients with burning pain at the vaginal opening and “vaginal pain” with intercourse often see many doctors as they or unable to obtain lasting relief, or even receive a clear diagnosis. As more doctors are becoming familiar with localized provoked vulvodynia, misdiagnosis is declining. However, it still may not be uncommon for both a doctor and patient to become frustrated over the persistent symptoms of LPV despite their best efforts.
In many cases, doctors will first misdiagnose a woman as having chronic or recurrent “yeast infections,” or candidiasis. The temporary response with antifungal medications to eliminate yeast may mislead both the doctor and patient to believe the problem is primarily yeast. Repetitive failed treatments lead to frustration and anxiety, worsening the symptoms, as stress has been identified as a trigger for making LPV worse. (8)
However, just because stress and lack of sleep, due to work, family life, or financial reasons may make the symptoms worse, it does not mean the problem is in a woman’s head. There are very real inflammatory changes within the tissue of the vulvar vestibule. The inflammatory changes are similar to those seen in allergies, such as mast cell and B cell infiltration, and the production of antibodies. (9 – 12) In fact, there is an association of inhalant allergies and localized provoked vulvodynia. (13)
 In some cases of treating women with localized provoked vulvodynia I was able to help them resolve the burning, and on examination the localized tender areas in the vulvar vestibule had mostly resolved. However, when they attempted to have sex they would still experience pain. In some cases, the pain at the opening was due to the development of developed vaginismus. Not only were these women not lubricating due to not being aroused, but understandably they were unable to relax to allow for penetration.
In some cases of treating women with localized provoked vulvodynia I was able to help them resolve the burning, and on examination the localized tender areas in the vulvar vestibule had mostly resolved. However, when they attempted to have sex they would still experience pain. In some cases, the pain at the opening was due to the development of developed vaginismus. Not only were these women not lubricating due to not being aroused, but understandably they were unable to relax to allow for penetration.
Vaginismus is a subconscious tightening or contraction of the muscles surrounding the vaginal opening, which can make sexual intercourse painful. Vaginismus occurs due to extreme fear or anxiety, which is brought on by beliefs, or a consequence to physical or psychological trauma. It is understandable that vaginismus would develop in a woman who always experiences pain with intercourse. It takes time and focused relaxation exercises to help eliminate this consequence.
The Frustration
Women with vulvar vestibulitis usually came to me misdiagnosed with chronic, recurrent yeast infections. They were frustrated, their husbands were frustrated, and they felt there was something wrong with them because they just weren’t getting better and could not tolerate intercourse. They were told to “get over it,” or it was “in their heads.”
Vaginal creams used to treat yeast infections usually cause burning pain in women with localized provoked vulvodynia. So when women with LPV are treated with a vaginal yeast cream they are confused and frustrated with burning that gets worse, when it “supposed to be getting better.”
Now whenever I hear that a woman is suffering from chronic yeast infections I know that vulvar vestibulitis, or localized provoked vulvodynia (LPV), is the most likely problem, as very few women have true chronic yeast infections (as opposed to recurrent yeast infections).
Many women who have been diagnosed by self or their doctor as having chronic yeast infections are often reluctant to give up that diagnosis, as they often have spent years managing chronic yeast infections with mild-to-moderate success. However, since management of vulvar vestibuilits involves minimizing the yeast population that normally exists within the vagina, these women are a step ahead of the game in knowing how to do that.
Yeast in the Vagina
 Yeast is normally found in the vagina. The overgrowth of yeast can cause irritation and itching that indicates the presence of a yeast infection. However, LPV is usually not accompanied by itching, but rather, mild to extreme burning pain, as well as pain with attempted penetration or other causes of pressure to the affected area. In those with LPV, normal levels of vaginal yeast can irritate the already sensitive, irritated areas within the vestibule.
Yeast is normally found in the vagina. The overgrowth of yeast can cause irritation and itching that indicates the presence of a yeast infection. However, LPV is usually not accompanied by itching, but rather, mild to extreme burning pain, as well as pain with attempted penetration or other causes of pressure to the affected area. In those with LPV, normal levels of vaginal yeast can irritate the already sensitive, irritated areas within the vestibule.
A change in the vaginal environment or bacteria-yeast ratio caused by hormonal fluctuations, intercourse, oral sex, and antibiotics can worsen the symptoms. Women without LPV can tolerate, and are completely unaware of a slight overgrowth of vaginal yeast. However, women with LPV are extremely sensitive to normal amounts of vaginal yeast, let alone an overgrowth. For women suffering with LPV it is important to maintain a healthy vaginal microbiome with normal bacterial and yeast flora and ratios. Overall, there should be no difference in the microbiome population of women with and without localized provoked vulvodynia. (14)
Part of the treatment and management of LPV includes minimizing vaginal yeast levels below normal. Oral anti-fungal medications, such as Diflucan, are convenient and effective for keeping candida yeast levels below normal. The reduction of yeast reduces secondary irritation, and therefore reduces symptoms of LPV. It is important to remember that anti-fungal medications are NOT the cure for LPV, and if the root cause for burning and pain with LPV is not addressed the symptoms will return as soon as the effect of the anti-fungal medication is over.
Estrogen Levels
 Dips in blood estrogen levels can exacerbate the symptoms of localized provoked vulvodynia. During the ten or so days prior to woman’s period there is a relative decline in estrogen blood levels compared to the peak at ovulation. The decline of estrogen has effects on the brain, triggering emotional premenstrual symptoms, such as anger, anxiety, and moodiness, as well as effects on the vulva and vaginal tissues. The relative lower estrogen levels prior to one’s period increases the sensitivity of the pain receptors in the vulvar vestibule to women with LPV.
Dips in blood estrogen levels can exacerbate the symptoms of localized provoked vulvodynia. During the ten or so days prior to woman’s period there is a relative decline in estrogen blood levels compared to the peak at ovulation. The decline of estrogen has effects on the brain, triggering emotional premenstrual symptoms, such as anger, anxiety, and moodiness, as well as effects on the vulva and vaginal tissues. The relative lower estrogen levels prior to one’s period increases the sensitivity of the pain receptors in the vulvar vestibule to women with LPV.
Similarly, the dramatic drop in estrogen levels after a baby is born or at menopause is also associated with both emotional and physiological changes, and can worsen the symptoms of vulvar vestibulitis. If fact, it is after pregnancy that many cases of vulvar vestibulitis first presents. A woman may have never had burning vaginal pain with intercourse until after childbirth. Also, the relative decline in estrogen seen at the onset of menopause may be the trigger for LPV, though this is less common than LPV arising during a woman’s reproductive years.
Free Radical Oxidative Stress Theory
We know that there is inflammation similar to an allergic reaction or hypersensitivity in the vulvar vestibular tissues in women with LPV. Also, as mentioned earlier, we know that chemical pollutants, such as dioxin from chlorine and other sources, irritate this tissue. Inflammation involves oxidative stress, as does an allergic reaction. And, dioxin causes oxidative free radical damage within the body. With both inflammation and chemical pollutants increasing free radical oxidative damage, I easily came to the conclusion that antioxidants could be used to blunt or prevent oxidative damage and inflammation.
The omega-3 fatty acids are needed for many functions in the body, including the integrity of cell membranes. DHA and EPA are the two most important omega-3 fatty acids. EPA has been shown to protect the cells from dioxin toxicity. (15)
Grape seed extract, turmeric extract, and many other antioxidants, work together to neutralize free radicals to inhibit oxidative damage better together than any individual antioxidant. They also block the Cox 2 enzyme involved in the inflammatory response. I have had great success using the antioxidants for allergies and asthma, and found great results in many women with LPV.
 Vitamins, minerals, antioxidants, and omega-3 fatty acids became an important part of my management protocol for localized provoked. Not all supplement brands work well, I know because I had many patients try various brands. Invariably, they had the best results with the quality brand I recommended. The science backed up what I recommended, and it was confirmed to be right by the results my patients experienced.
Vitamins, minerals, antioxidants, and omega-3 fatty acids became an important part of my management protocol for localized provoked. Not all supplement brands work well, I know because I had many patients try various brands. Invariably, they had the best results with the quality brand I recommended. The science backed up what I recommended, and it was confirmed to be right by the results my patients experienced.
I recommend high doses of a wide array of powerful antioxidant nutrients, and in particular a grape seed extract. All of these are completely safe, and are also beneficial in reducing the risk of cancer, heart disease, diabetes, dementia, and arthritis. Therefore, a person who uses these consistently will not only help reduce their symptoms of LPV, they will enjoy benefits throughout their body.
Conclusion
Vulvar vestibulitis is now known as localized provoked vulvodynia (LPV). It is a far too common problem affecting women, and the prevalence appears to be increasing. The increase may be due to the increasing exposure to environmental toxins in our food, water, and air. Chlorine in pools, household water supply, laundry, and used to whiten feminine hygiene products and toilet paper negatively affects LPV.
Localized provoked vulvodynia is a difficult and frustrating condition to treat and manage. The tissue is irritated by the normal presence of yeast in the vagina, and exacerbated by stress and anxiety. The disruption of sexual intercourse affects personal relationships, so it requires a great deal of patience and the need for couples to be creative in their love making so not to lose the important physical bonding.
The best that anyone can do is to decrease exposure to toxic chemicals by drinking reverse osmosis water, avoiding chlorinated pools, not using bleach on underwear, avoiding bleached-whitened feminine products and toilet paper, and consistent use of broad-spectrum of quality vitamins, minerals, antioxidants, and omega-3 fatty acids.
Below are the instructions I gave to my patients.
Dr. Ladd’s Guidelines for Managing Localized Provoked Vulvodynia
 Nutritional supplementation according to my protocol below.
Nutritional supplementation according to my protocol below.- Ten glasses of water per day (distilled, reverse osmosis, or micro filtered; No chlorine)
- Drink 2 glasses of water first thing in morning at least 30 minutes before eating or drinking anything.
- Obtain prescription for the antifungal, Diflucan®. Take 150 mg tablets once weekly, or every-other week, depending upon severity. (Take the liver support supplement if taking Diflucan) This is not to treat a vaginal yeast infection, but rather to decrease the normal levels of yeast that inhabit the vagina in order to decrease the compounded irritation. This is an important concept for the patient and her doctor to understand.
- Do not use antifungal creams; they will only perpetuate the problem, making it worse due to the chemicals within creams, such as propylene glycol. It must be an oral treatment.
- If any vaginal creams are used, they must not contain propylene glycol, butylene glycol, phthalates, parabens, formaldehyde, fragrances, etc.
- Apply “Dr. Ladd’s Vulvar Vestibulitis Oil Regimen,” which will soothe the vulvar vestibule (opening of the vagina). Apply the oil mixture 3 to 5 times per day and immediately after intercourse. The more often you apply the oil mixture the better it will be. It is especially necessary during flare-ups, and immediately after intercourse. Spread the labia minora, and apply with your fingers. Get the oil up between the labia minora. You don’t need to go up more than one inch.
- Prepare “Dr. Ladd’s Vulvar Vestibulitis Oil” mixture as follows, with a range of the essential oils allowable, as shown:
- Jojoba oil ½ cup,
- Tea tree oil approx. ¼ tsp. (1.0 – 1.5 ml)
- German chamomile oil approx. ½ tsp. (2.5 – 3.0 ml)
- No bleach-whitened feminine paper products (tampons, pads). Chlorine is your enemy with this localized provoked vulvodynia.
- Use unbleached pads, such as “Playtex Naturals” or “Natracare.” You may use feminine products that have been whitened with hydrogen peroxide. Avoid tampons; use pads.
- Do not use toilet paper whitened by bleaching either. Use a toilet paper that is not whitened or whitened with hydrogen peroxide.
- Do not swim in pool or sit in hot tub that has chlorine added to the water. Bromine is fine, but not chlorine
- If possible, get home de-chlorinator plumbed in, so that you can bathe and shower in water that does not have chlorine. At minimum, get a showerhead de-chlorinator.
- Do not use chlorine in wash with underwear.
- Do not use any feminine hygiene sprays.
- Do not use Astroglide, KY Liquid, or any sexual lubricant that contains any glycerin, propylene glycol, butylene glycol, or parabens. You may use regular KY Jelly, or equivalent. My suggestion is to use a non-toxic, natural lubricant as from Blossom Organics®.
- Avoid harsh skin soap and laundry detergents on pants or underwear that will be touching the vulva.
- Skin cleansers: Use a clean, non-toxic shower gel on your body, and a gentle, non-soap cleanser that you can use daily on the vulva.
- No Laundry detergents with bleach. Underwear should be put through a double rinse cycle, preferably in non-chlorinated water.
- Do not use fabric softeners, and do not use cling free sheets for your underwear.
- No aspartame (“NutraSweet” & “Equal”), which is found in diet drinks and the sweetener in the blue packets, or sucralose (“Splenda”) found in the yellow packets. Stevia is the best alternative to sugar.
- Keep caffeine and alcohol to a minimum.
- No foods high in nitrate preservatives, such as preserved meats (pepperoni, luncheon meats, etc.)
Supplement Protocol FOR Localized Provoked Vulvodynia (Vulvar Vestibulitis)
 The micronutrients referenced in the various protocols below, combined with the Guidelines above, will do more to help a woman with localized provoked vulvovdynia than any other non-surgical procedure available.
The micronutrients referenced in the various protocols below, combined with the Guidelines above, will do more to help a woman with localized provoked vulvovdynia than any other non-surgical procedure available.
Improvements will be a gradual process, and it will wax and wane, particularly with stress and one’s menstrual cycle. If results are not satisfactory, then increase the doses to a higher protocol, and pay strict attention to the guidelines above.
Please read medical disclaimer below, and consult your health care professional prior to acting upon information provided in the article, protocol, or website.
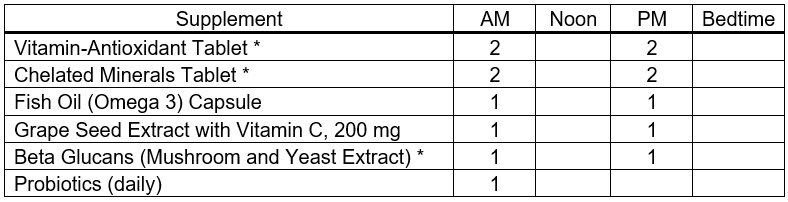
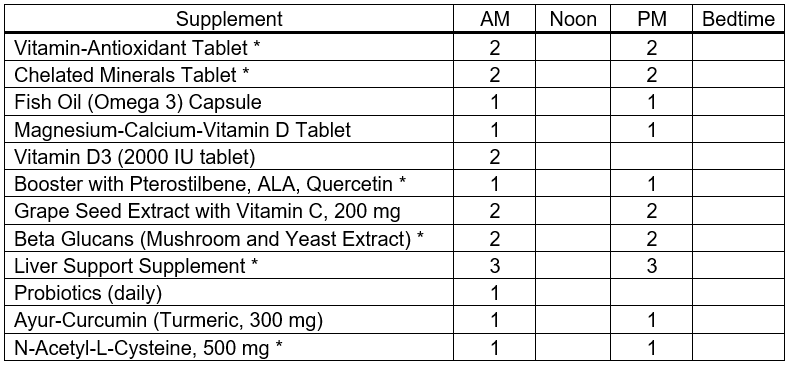
Minimal Protocol for Localized Provoked Vulvodynia
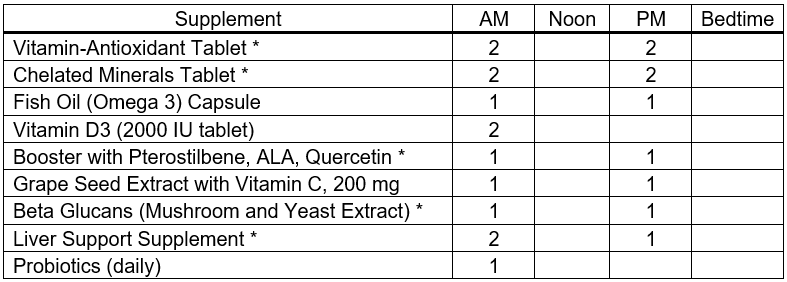
Basic Protocol for Localized Provoked Vulvodynia
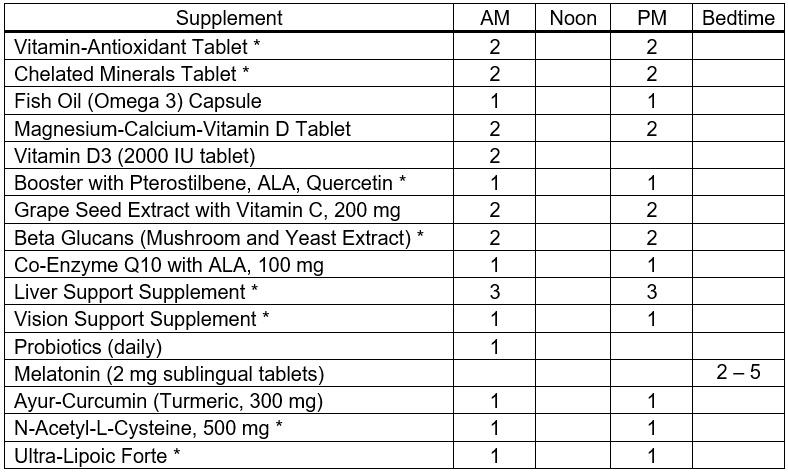
Average Protocol for Localized Provoked Vulvodynia
Advanced Protocol for Localized Provoked Vulvodynia
- AM: With, or after breakfast
- Noon: At lunchtime with food, or shortly thereafter
- PM: Late afternoon with food, or at, or after dinner
- Booster Antioxidant Supplement, with each tablet providing 50 mg Pterocarpus marsupium extract (containing pterostilbene), 10 mg Olive Fruit Extract, 75 mg alpha lipoic acid (ALA), and 60 mg Quercetin.
- Liver Support Supplement, providing Milk Thistle Extract, N-Acetyl-L-Cysteine, Alpha-Lipoic Acid, Broccoli Extract, Turmeric Extract (Curcumin), Olive Extract, Green Tea Extract, Biotin
- Beta Glucan Supplement, derived from the extracts of the Reishi and Shiitake Mushroom, as well as Baker’s Yeast Extract.
- Vision Support Supplement, providing lutein, zeaxanthin, bilberry extract, and zinc.
- Probiotics, providing Lactobacillus rhamnosus LGG® and Bifidobacterium BB12®, every other day or daily.
- Ayur-Curcumin (Turmeric, 300 mg), N-Acetyl-L-Cysteine (NAC, 500), and Ultra Lipoic Forte, can all be purchased from Douglas Labs by first creating a customer account by CLICKING HERE. (If this link does not work for you, simply type “douglaslabs.com/patient-account” into a new browser tab.) Please use Referral Code 2074214. After setting up your customer account, simply search for the product(s) by name.
Ingredients that I like to see provided collectively by vitamin-antioxidant & chelated mineral tablets
Vitamin A, mostly as Beta Carotene
Vitamin C
Vitamin D3
Vitamin E
Vitamin K (K1 & K2)
B-Complex Vitamins
Curcumin (turmeric extract)
Quercetin
Green Tea Extract
Olive Extract
Rutin
Resveratrol
Choline
Lutein
Lycopene
N-Acetyl-L-Cysteine (NAC)
Calcium
Magnesium
Iodine (as potassium iodide)
Zinc
Selenium
Copper
Manganese
Chromium
Molybdenum
Including Ultra Trace Minerals
Medical Disclaimer
Information on this website, written, spoken, or in any other communication by Dr. Ladd McNamara or any other information or reference is for informational purposes only. The information provided on this website is a result of years of practice, experience, and study by the author. This information is not intended as a substitute for the advice provided by someone’s personal licensed physician or other healthcare professional, or any information contained on or in any product label or packaging. Do not use the information on this website, or any other form of communication from Dr. Ladd McNamara or the Dr. Ladd VIP Program, for diagnosing or treatment of a health issue or disease, or for the prescribing of medication or the use of supplementation without a discussion with your licensed health professional first. At best, the information provided on this website is only meant to supplement information provided by your own doctor or health professional, not to replace medical advice. The information from this website is not meant to cover all possible uses, precautions, interactions or possible adverse effects of nutritional supplements with or without medications, or in conjunction with specific medical conditions. The information from this website may not fit your specific health circumstances. Never delay seeking medical care or disregard advice from your health care professional because of information you have received directly or indirectly from this website, from the Dr. Ladd VIP Program, or from Dr. Ladd McNamara himself. Always speak with your physician or other healthcare professional before making any changes to your medication or embarking on a nutritional, herbal or homeopathic supplement program, or before using any treatment for a health concern. If you have, or suspect that you have, a medical problem, contact your health care provider promptly. Do not disregard professional medical advice or delay in seeking professional advice because of something you have read or heard on this website, or due to any other information from Dr. Ladd McNamara or his representatives. Information provided on this website or the V.I.P. Program, and the use of any products or services mentioned on this website (or as a result of information provided this program, article, or website) by you DOES NOT create a doctor-patient relationship between you and Ladd McNamara, M.D. Information and statements regarding dietary supplements have not been evaluated by the Food and Drug Administration and are not intended to diagnose, treat, cure, or prevent any disease.
References
- De Andres J, et al. Vulvodynia—An Evidence-Based Literature Review and Proposed Treatment Algorithm. Pain Practice 2016 Feb;16(2):204-236.
- Tommola P, et al. Long-term well-being after surgical or conservative treatment of severe vulvar vestibulitis. Acta Obstet Gynecol Scand. 2012 Sep;91(9):1086-93.
- Tommola P, et al. Long-term follow up of posterior vestibulectomy for treating vulvar vestibulitis. Acta Obstet Gynecol Scand. 2011 Nov;90(11):1225-31.
- Huang Q, et al. Dioxin-like rather than non-dioxin-like PCBs promote the development of endometriosis through stimulation of endocrine-inflammation interactions. Arch Toxicol. 2017 Apr;91(4):1915-1924.
- Vabre P, et al. Environmental pollutants, a possible etiology for premature ovarian insufficiency: a narrative review of animal and human data. Environ Health. 2017 Apr 7;16(1):37.
- Smarr MM, et al. Endocrine disrupting chemicals and endometriosis. Fertil Steril. 2016 Sep 15;106(4):959-66.
- Martínez-Zamora MA, et al. Increased levels of dioxin-like substances in adipose tissue in patients with deep infiltrating endometriosis. Hum Reprod. 2015 May;30(5):1059-68.
- Ehrström S, et al. Chronic stress in women with localised provoked vulvodynia. J Psychosom Obstet Gynaecol. 2009 Mar;30(1):73-9.
- Falsetta ML, et al. A review of the available clinical therapies for vulvodynia management and new data implicating proinflammatory mediators in pain elicitation. 2017 Jan;124(2):210-218.
- Seckin-Alac E, et al. Elevated tissue levels of tumor necrosis factor-α in vulvar vestibulitis syndrome. Clin Exp Obstet Gynecol. 2014;41(6):691-3.
- Tommola P, et al. Activation of vestibule-associated lymphoid tissue in localized provoked vulvodynia. Am J Obstet Gynecol. 2015 Apr;212(4):476.e1-8.
- Theodoropoulos DS, et al. Inhalant allergy compounding the chronic vaginitis syndrome: characterization of sensitization patterns, comorbidities and responses to sublingual immunotherapy. Arch Gynecol Obstet. 2016 Sep;294(3):541-8.
- Landry J, et al. Repeated hapten exposure induces persistent tactile sensitivity in mice modeling localized provoked vulvodynia. PLoS One. 2017 Feb 3;12(2):e0169672.
- Jayaram A, et al. The bacterial microbiome in paired vaginal and vestibular samples from women with vulvar vestibulitis syndrome. Pathog Dis. 2014 Dec;72(3):161-6.
- Palanisamy K, et al. Eicosapentaenoic acid prevents TCDD-induced oxidative stress and inflammatory response by modulating MAP kinases and redox-sensitive transcription factors. Br J Pharmacol. 2015 Oct;172(19):4726-40.
- De Andres J, et al. Vulvodynia—An Evidence-Based Literature Review and Proposed Treatment Algorithm. Pain Practice 2016 Feb;16(2):204-236.
- Tommola P, et al. Long-term well-being after surgical or conservative treatment of severe vulvar vestibulitis. Acta Obstet Gynecol Scand. 2012 Sep;91(9):1086-93.
- Tommola P, et al. Long-term follow up of posterior vestibulectomy for treating vulvar vestibulitis. Acta Obstet Gynecol Scand. 2011 Nov;90(11):1225-31.
- Huang Q, et al. Dioxin-like rather than non-dioxin-like PCBs promote the development of endometriosis through stimulation of endocrine-inflammation interactions. Arch Toxicol. 2017 Apr;91(4):1915-1924.
- Vabre P, et al. Environmental pollutants, a possible etiology for premature ovarian insufficiency: a narrative review of animal and human data. Environ Health. 2017 Apr 7;16(1):37.
- Smarr MM, et al. Endocrine disrupting chemicals and endometriosis. Fertil Steril. 2016 Sep 15;106(4):959-66.
- Martínez-Zamora MA, et al. Increased levels of dioxin-like substances in adipose tissue in patients with deep infiltrating endometriosis. Hum Reprod. 2015 May;30(5):1059-68.
- Ehrström S, et al. Chronic stress in women with localised provoked vulvodynia. J Psychosom Obstet Gynaecol. 2009 Mar;30(1):73-9.
- Falsetta ML, et al. A review of the available clinical therapies for vulvodynia management and new data implicating proinflammatory mediators in pain elicitation. 2017 Jan;124(2):210-218.
- Seckin-Alac E, et al. Elevated tissue levels of tumor necrosis factor-α in vulvar vestibulitis syndrome. Clin Exp Obstet Gynecol. 2014;41(6):691-3.
- Tommola P, et al. Activation of vestibule-associated lymphoid tissue in localized provoked vulvodynia. Am J Obstet Gynecol. 2015 Apr;212(4):476.e1-8.
- Theodoropoulos DS, et al. Inhalant allergy compounding the chronic vaginitis syndrome: characterization of sensitization patterns, comorbidities and responses to sublingual immunotherapy. Arch Gynecol Obstet. 2016 Sep;294(3):541-8.
- Landry J, et al. Repeated hapten exposure induces persistent tactile sensitivity in mice modeling localized provoked vulvodynia. PLoS One. 2017 Feb 3;12(2):e0169672.
- Jayaram A, et al. The bacterial microbiome in paired vaginal and vestibular samples from women with vulvar vestibulitis syndrome. Pathog Dis. 2014 Dec;72(3):161-6.
- Palanisamy K, et al. Eicosapentaenoic acid prevents TCDD-induced oxidative stress and inflammatory response by modulating MAP kinases and redox-sensitive transcription factors. Br J Pharmacol. 2015 Oct;172(19):4726-40.
All materials on this website, written, audio, visual, are copyrighted by Ladd McNamara, Inc., and are not to be distributed, duplicated, shared, posted to another website or social media sites (including Facebook, etc.), except for under the Terms of Use for sharing approved articles and videos.
As a VIP member, you agree that you will NOT share any written, audio, video, or any other proprietary materials from this website with those in your organization, other associates, or team members; and that you will only share approved articles/protocols and videos with your OWN PERSONAL & IMMEDIATE customers, clients, and prospective customers/clients. Doing so, would result in the loss of your Dr. Ladd VIP membership without a refund.
Thank you for your honesty and integrity.
About the Dr. Ladd VIP Program
There are many more articles on various subjects, as well as videos on health concerns, along with specific nutritional supplement protocols for managing health concerns and disease. Of course, this is all for informational purposes, and not to be taken as medical advice. (See medical disclaimer above.) Please learn more at www.drladdvip.com.
Please read about the benefits of being a Dr. Ladd VIP Member. It is a subscription-based personal program to better your health, energy, and passion for life, and for helping others. This program includes on-going support for yourself, and as you help customers and clients with your health enterprise.
Do you have a need to understand how NUTRITIONAL SUPPLEMENTS can benefit the health of people suffering from any number of chronic diseases; such as Heart Disease, Cancer, Diabetes, Arthritis, Dementia, Lyme Disease, Autoimmune Diseases, and Many More!
- Do you have a need for SUPPLEMENT PROTOCOLS as to what specific supplement combinations to use?
- How about WHY SUPPLEMENTS? How do you chose a QUALITY BRAND?
- Do you have a need to BETTER ASSIST CUSTOMERS in making a good decision?
- How about ON-GOING SUPPORT for ON-GOING QUESTIONS?
- How about YOUR PERSONAL HEALTH, and/or Your PERSONAL RELATIONSHIPS?
Happiness and Health includes not only being free of disease, but passionately engaged in a relationship, in life, and in helping others! It means living with less stress, more fun, and activity.
The Dr. Ladd VIP Program is about Vitality, Intimacy, and Passion, being balanced in all aspects of life, and helping others to get there too.
 Please read more at www.drladdvip.com, and take advantage of the Video Courses, the Supplement Protocols, Articles, Downloadable PDFs, and Dr. Ladd VIP Facebook Community and Support. “Have me in your back pocket” by becoming a VIP Member Today!
Please read more at www.drladdvip.com, and take advantage of the Video Courses, the Supplement Protocols, Articles, Downloadable PDFs, and Dr. Ladd VIP Facebook Community and Support. “Have me in your back pocket” by becoming a VIP Member Today!
If you are not a VIP member, please subscribe to my email list. If you are already a VIP member, no need to subscribe to the email newsletter list. Thank you.
dr. ladd
Please learn more about the Dr. Ladd VIP program here: www.drladdvip.com.
Please Subscribe to Dr. Ladd’s Email List
Receive health and website updates, as well as information on upcoming FREE health-related webinars.
All information, written or video, is copyrighted by Ladd McNamara, Inc., and is not to be shared, duplicated, or posted to other websites or social media platforms without express permission from Ladd McNamara, M.D. Thank you.
Dr. Ladd’s V.I.P. Program and Website is Owned and Operated by Ladd R. McNamara, M.D. and Ladd McNamara, Inc., a California corporation.
